Clinical Evidence
Theoretical underpinning to ex-vivo functional testing
There is an increasing acceptance that a “one-size-fits-all” approach to all aspects of medicine is inappropriate and insufficient.
Taking cancer as an example, the press has been full of stories about the potential of personalised therapy to dramatically increase response rates (links to references). In line with this, there is a growing acceptance that choosing a therapy purely based on the organ in which a cancer first arose, while ignoring the molecular characteristics of that particular tumour, is illogical.
Likewise, pharmaceutical companies are able to decide which cancer types a specific drug is registered for; a decision which is often based on which markets they wish to address with which drugs at which times. This decision-making process is complex. Yes, it involves good logical science, but it is also influenced by non-scientific factors such as market size, overall drug portfolio, predicted price point achievable, and so on.
Because each cancer arises from a unique set of mutations, the sensitivities of different tumours to different drugs is highly individualised and unpredictable. Drug sensitivities between tumours found in the same organ vary dramatically, and the most effective drug for treating a cancer of the ovary, for example, may in fact turn out to be one licensed for use in, say, lung cancer. Just because a drug is not generally used in a certain cancer type, this does not mean that it will always be ineffective in individuals with that cancer type. This is true even if there have been clinical trials demonstrating that the treatment has no utility for the majority of patients.
We are in fact in a “golden age” of cancer therapy right now, with more drugs available than ever. Some of these are dramatically effective in certain patients. However, these drugs tend to work in only a small proportion of individuals. The current challenge is therefore choosing which drugs are best for each patient.
If we could discover a way of finding the best drug for each patient, outcomes would be dramatically improved even without the development of new drugs; by using what we have now more effectively.
It is this matching of drugs to patients that Imagen Therapeutics is striving for.
There are two basic approaches to better matching of drugs to patients:
- The “genetic” approach
- Functional testing – Imagen Therapeutics’ basic methodology
The genetic approach works as follows:
- Collect data on the genetic mutations in lots of patients’ cancers
- Collect data on how well those patients responded or didn’t respond to particular drugs
- For future patients, attempt to predict sensitivities by comparing each patients’ mutations against the database to see what drugs are suggested
What are the pitfalls of the genetic approach?
There are literally tens of thousands of possible mutations. Each cancer may have a few or many of these and the relationship between these mutations and how drugs work is not well understood. Having one fewer or one more mutation may affect the biology of the cancer cell such that its sensitivities to different drugs is very different. It can therefore be difficult to predict drug sensitivities by comparing a patient’s mutation against a standard database; the mutational possibilities are too vast.
The Imagen approach
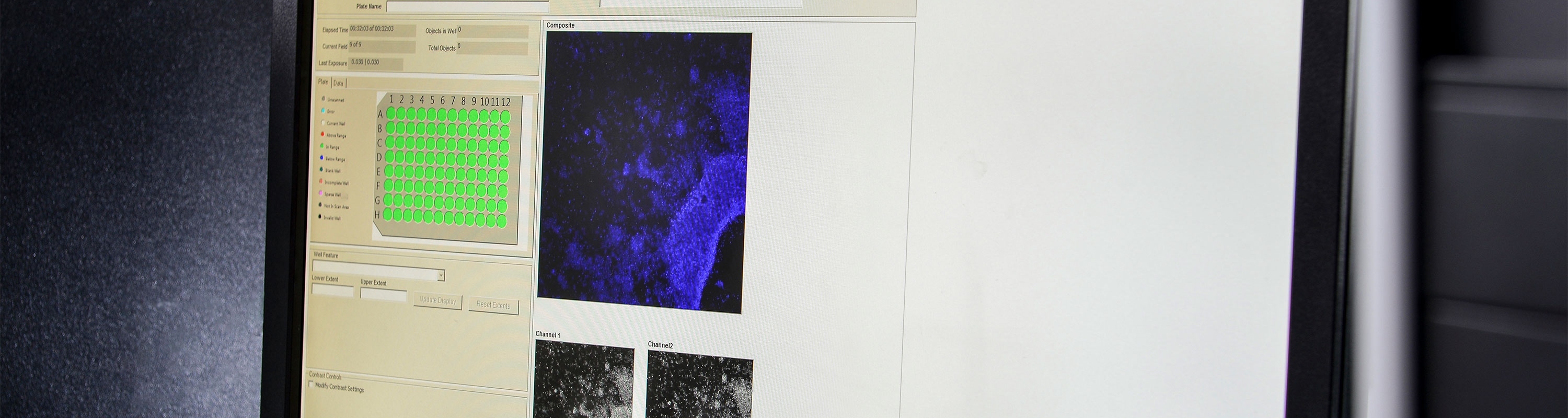
Imagen Therapeutics perform a functional test, which is often termed a phenotypic screening approach. The approach is concerned only with examining the overall “functioning” of the cell under certain scenarios – in this case what they do when exposed to different drugs.
We take a sample of the patient’s cancer and expose the cells to a variety (up to 56) of different drugs for 72 hours and measure their cytotoxic effects.
This type of testing is vastly simpler than genetic approaches as it is entirely unconcerned with the inner biochemical pathways of the cancer cells. Instead, it focuses on determining what makes the cancer cells die.
In some respects, this is similar to the way in which antibiotics are selected for treating infection – a sample of the bacteria causing the infection is treated with various drugs to determine which is most lethal to the bacteria.
This simpler approach provides a number of benefits:
- ACCURATE – direct measure of cell death
- FAST – results available within 2 weeks
- COMPREHENSIVE – routinely produce detailed information on up to 56 different chemotherapies including drug combinations
- TRULY PERSONALISED – tested on samples derived directly from your patient
- Results tell the treating oncologists which drugs are killing the cancer cells, as well as the minimum dose at which a drug is effective (potency data)
- The provision of potency data potentially means that an oncologist can also form a view as to the possible therapeutic window a particular treatment might have in relation to unpleasant side effects
Previous experience with functional testing
Given it seems so obvious, surely it must have been tried before, and if it isn’t currently widely used doesn’t that mean that it won’t work?
The history of functional testing goes right back to the 1980s and 1990s, when there were many studies assessing the role of such technology. Broadly, most studies showed a tendency to result in higher response rates with a general view that “further testing was required”.
The concentration of research into genetics from the mid-90s onwards effectively put a brake on the further examination of functional testing as it was assumed (incorrectly as it turned out) that by understanding the genetic basis of cancer, the molecular aberrations causing uninhibited growth of each cancer could be easily identified and targeted.
Imagen Therapeutics’ test its origins in earlier attempts at functional testing, but with a few very important differences. These differences ensure our test is better than earlier attempts to personalise chemotherapy using functional assays.
Assay technology
Many early studies used assay technologies that are greatly inferior to techniques used by Imagen Therapeutics. These included MTT and ATP assays, neither of which measure cell death directly but rather an average metabolic reading that is assumed to be proportional to the number of cells present. In these types of assay, agents that suppress cellular metabolism or cell division, without inducing cell death, will give a false positive reading.
In contrast, Imagen Therapeutics’ test provides a direct measure, meaning that it can separately determine whether a compound’s action induces cell death or inhibits cell growth. This is possible because we directly image the cells, meaning that we can delineate cytotoxic from cytotrophic effects.
Because of the technology we use, Imagen Therapeutics is able to work with minimal amounts of fresh tissue. This means that we can test many drugs at different doses, without having to culture cells to produce greater quantities – something which has been criticised in the past as leading to “phenotypic drift”. This is a phenomenon whereby the underlying biological characteristics vary over successive generations.
We also preserve the in vivo characteristics of the cancer cells by not culturing the cells with animal blood serum. Instead, we use our own defined and patented tissue culture solutions. In some cases, we can create an autologous assay whereby we culture the patient’s cells in their own blood serum (Patent Pending), thus largely preserving the growth factor profile that the cancer cells were exposed to in vivo.
The drugs tested
Any personalised therapy will only ever be as good as the best effective treatment under consideration for that cancer. In short, if none of the drugs work very well, then personalised chemotherapy offers the patient little benefit; all it is doing is identifying the “least bad” drug. Such an approach cannot translate into meaningful improvements in patient survival.
In general, the number of treatment options that were examined during the 1990s studies was very limited and this is another reason why the data produced was a little underwhelming. The big change since then is the development of many more potential chemotherapies, making the potential utility of personalised approaches much more acute. However, it is important that we learn an important lesson from this earlier research work.
Using a personalised chemotherapy test to distinguish which is the best available treatment out of all the therapies that are licensed for a particular cancer is likely to be a flawed strategy in most cancers. In cancers which carry a poor prognosis, by definition, none of the therapies are particularly effective. This means that the correct and accurate selection of even the best performing drug out of the licensed therapies is unlikely to result in any significant increase in patient survival.
Our contention is that a personalised therapy strategy will only be of real benefit to patients with poorly managed cancers if:
- the test examines the full range of treatments available, not just those licensed for the cancer in question; and
- the oncologist is able to select the best performing therapy, independent of whether there has been a trial showing benefit in cancer of that particular origin.
This is a major shift in the cancer treatment paradigm, but also one which is becoming more accepted at the current time.
Our data
Between 2013 and 2015, Imagen Therapetuics has processed many different cancer samples using our system.
In ovarian cancer, we compared the actual clinical response rates of patients to their next cycle of chemotherapy with the chemosensitivities we predicted. (Note: this was a match-up exercise to test the predictive value of our test; we did not influence treatment).
Of the 28 patients for whom we have had clinical follow-up data, we correctly predicted the response to the next chemotherapy they received in all but one case.
Of the 28 patients, 21 patients did NOT respond to their next cycle of chemotherapy, and we predicted that this would be the case in all 21 patients.
Eight patients DID respond to their next cycle. We predicted that this would be the case in seven of the eight cases.
Our clinical partners are currently auditing this preliminary data prior to publication.
During this auditing process, we found that in one patient:
- We predicted that she would not respond to a paclitaxel, carboplatin combination. As expected, her Ca125 levels and CT scan data indicated that the tumour had increased in size (progressive disease) during this treatment.
- Later, she was switched to carbocaelyx (a doxorubicin, carboplatin combination). Our screening data had clearly indicated that she would respond to doxorubicin, and, as expected, this second line treatment was very effective against her cancer.
These data mean that Imagen Therapeutics correctly identified not only drugs that would not work for this patient but also predicted a drug that turned out to be effective.
An additional point to note is that, within the 21 non-responders, our data suggested that several patients would have responded well, and in some cases, extremely well, to drugs which are not regarded as “standard of care” for the cancer type in question.
Imagen Therapeutics remains committed to helping improve cancer treatment outcomes for all cancer sufferers.
If you would like more information about our company or feel you can support our experimental aims then please do not hesitate to get in contact.
Ongoing projects and news:
- We have performed several experiments examining the concordance of our data to that provided to us by several PDX suppliers. Broadly, our data suggests that our test is measuring the same thing as the PDX studies; that is to say, our chemosensitivity predictions match those known sensitivities of the tumour samples
- We have processed a number of fresh, human samples without difficulty. These produce good, clear drug signatures, which are as good as those from ascites fluid
- Finally, later this year we expect to be commencing a trial of our technique with NHS paediatric oncologists in the treatment of a range of recurrent childhood cancers